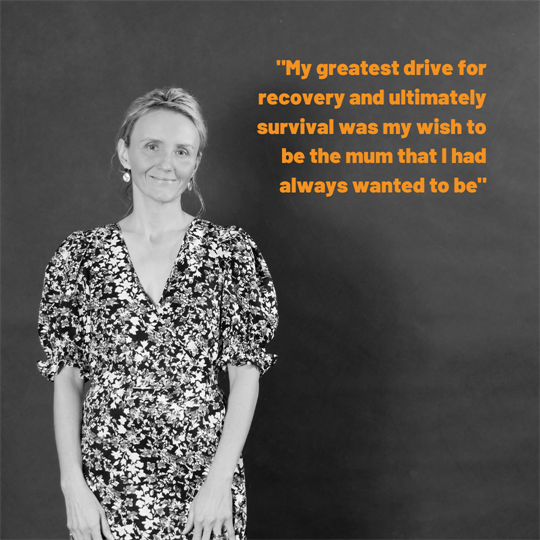
Diagnosed with bowel cancer at age 38, Sally’s two young boys were by her side when she was delivered the news, “I’m sorry you have Cancer”. The Sunshine Coast nurse had major bowel surgery, the cancer was caught early, and Sally did not need chemotherapy.
Sally’s 12-month recovery was littered with many hurdles and she did it all while caring for an 18-month-old and three-year-old with her husband. Her fear of being a “sick mum” to her two beautiful sons turned into her greatest motivator to get well.
In an interview with Bloomhill, she highlights the challenges and triumphs of parenting through cancer. Sally wants every parent to know that they are not alone, “your best is good enough”, mindset is key, and that as long as your children are safe and loved they will grow and thrive regardless of how your lifestyle may change while you are unwell.
June 2021
Hi, I’m Sally and I’m sharing my story because I want parents with cancer to know that they are not alone. I hope that others can learn from my experiences to make their journey a little easier.
When I was first diagnosed with cancer, I had an 18-month-old and three-year-old. My greatest drive for recovery and ultimately survival was my wish to be the mum that I had always wanted to be. I wanted to be there for my children and for my husband.
Through my diagnosis, I have discovered that the resources and support services for younger parents are lacking. A lot of patient information and funding is targeted at older adults.
I didn’t have a guide to ‘parent from the lounge’. I didn’t have a hint sheet on how to get myself and my children out to the park when I had nausea, fatigue and diarrhoea. I didn’t know that a trip to an unfenced park with a three meter climbing frame was a seriously bad idea!
On a day to day basis I learned from trial and error. I based each day on what did and didn’t work previously. I have since found that many parents with cancer find that their greatest recovery challenge is the juggle of being mum or dad through their treatment or recovery.
For most people, a cancer diagnosis will unleash a cascade of tumultuous emotions. For parents of young children, these emotions are amplified. There is not only yourself to consider, the care of your children needs to be prioritised. You cannot put your beautiful title of ‘mum or dad’ on hold while you recover. Patients always hear “you need to rest”. How do you prioritise rest and recovery when you have younger children?
The feelings of guilt and fear can become all-consuming. Guilt that you are not able to be there for your children because you are unwell and guilt that you are missing important family moments because you are in hospital or at home in bed. There is also a fear that your children and your partner will lose you, and even that your children will have long-term emotional effects from seeing you unwell. For some of us, there is also a grief. A grief for the loss of a ‘care-free’ future. Many people who’ve had cancer live with the worry that the cancer may return, involving long-term treatment regimes and many years of cancer surveillance appointments.
My beautiful boys are today very happy and thriving four and six-year-olds. I wish that I had someone to tell me back then on my hardest days, “Sally, your children are going to be just fine! Outsource whatever you can, say yes to all help, write a list of tasks you can delegate, say yes to additional day care, and prioritise your mindset. Shorter park plays, some extra TV and the occasional nutritional frozen meal is absolutely fine. You and your husband are doing your best- and your best is good enough”.
If you’re reading this, you probably found out recently you have cancer. Either that or you want to donate to Bloomhill so it can continue its support of people like me (please do!). I want you to know you’re not alone.
Bloomhill
I contacted Bloomhill early into my recovery, a couple of weeks after my surgery. I had heard from colleagues that Bloomhill was a fantastic organisation that supports cancer patients and their families, of all ages. I needed to connect with a team who really understood the emotional and physical needs of a cancer patient (at home). I needed advice on how to make my recovery easier so that I could get back to my life. I was so glad that I reached out to Bloomhill when I did. If you are thinking about contacting Bloomhill, do. They have an amazing team who are ready to support you.
“That’s not my story”
When I received my diagnosis and for about a week after my surgery I had no idea if I would survive or have my life shortened. I made the decision to stop searching Dr Google and to unfollow online cancer support groups until I was more resilient. I found the stories of young mums with end stage disease extremely sad. Women my age and younger, also with young children nearing the end of their life in my online cancer communities. I would think “that could have been me”, “will that be me?”. As I become stronger emotionally and physically (the two went hand in hand), I was able to tell myself “that’s not my story”. This became my mantra and I could be empathetic without being distressed (mostly). I share my story now because I want to provide an alternative to the negativity and tragic stories you’ll inevitably come across in your research.
I am extremely grateful that the cancer in my bowel was detected early and removed. I’m also conscious that many wonderful people – mothers and fathers included – have been lost to this disease. I want this letter to leave you feeling a warm hug, regardless of your situation, because in my experience people with cancer and their loved ones can’t have too many of those.
It started with stomach bloating
I had stomach bloating and intermittent stomach pain for about a month before I saw my GP. There was no bleeding, no persistent change in toilet habits and no weight loss. I don’t have a family history of bowel cancer. The amazing GP that saw me that day decided that I should have a colonoscopy and blood tests to ‘cover all bases’.
Because I didn’t have bleeding, I decided to wait about 6 weeks to have my colonoscopy. But… I had a voice in my head saying, “you really should do that colonoscopy”. It’s really important to listen to your intuition
After the colonoscopy the Gastroenterologist let me know that he’d removed a few polyps and was concerned about one of them. He let me know that one of the polyps was abnormal, and that the results of the biopsy were needed before we knew more. It was then that I was told that some of my bowel may need to be removed. I decided not to jump to worst case scenario and wait for the facts. I was young, healthy, lean and relatively (mum) fit. I was tired, which is normal for parents who have children. I did not expect to be diagnosed with bowel cancer three days later.
The advice that I would give today is, that if your GP recommends for you to have a colonoscopy- organise it straight away. The earlier that the abnormal cells are detected, the better your outcome. Early detection is the key.
‘You’ve got cancer’
Three days after my colonoscopy I had a missed call from my GP. When I listened to her voice message I knew that I had cancer. I rushed to the GP practice, and with my 18month-old and 3-year old by my side I was told that I had cancer. It was impossible to know what stage (how severe) the cancer was, what my prognosis was or what sort of treatment I would need. It was the most surreal experience of my life. I felt like time had stood still. I was watching my two little boys opening and closing clinic drawers, pulling paper off the examination table and asking the GP for a balloon. I tried to hide my crying and asked my GP “what am I going to do, I have two little boys that need me”. I was deeply shocked and taking in only snippets of information.
My GP asked me if I had supports, “because you really need them right now”. The truth was, yes and no. I had my wonderful husband, friends, and my parents were nearby but did I have the supports I needed? I didn’t know. I had no idea what would happen to my sons when I disappeared for surgery, let alone the recovery and whatever else lay ahead.
In the few days that followed, I would wake up and forget for a micro second that I had cancer. Those were treasured moments.
‘Rally the troops’ advice from my surgeon
At the time of my diagnosis I had been a nurse for 18 years. I had supported many patients through their cancer recovery, and I had been a by-stander to many sad stories. I knew that there were so many unknowns and everyone has a different experience. Everyone has their own story.
My husband came with me to meet the Surgeon. I still hadn’t really processed that seemingly overnight I had become a cancer patient, and here we were planning a major operation. The cancer type and severity could only be confirmed after the cancer cells were tested. We wouldn’t know for about a week after the operation if I would need chemotherapy. My surgeon discussed the surgery in detail and said to us “this is the time where I tell my patients to rally the troops”. Again, I cried and said “But I have two little boys, this can’t be happening”. I had about 10 days to prepare for my operation.
Project Bowel Cancer Survival
In the lead up to my surgery I went into project manager mode. I did as much bulk cooking as I could, organised extra daycare days, organised approvals for extra day care days through Centrelink, scheduled time off work, organised health insurance cover for my operation, and completed income protection paperwork through my super. The list seemed never ending.
In between completing all of the before surgery ‘tasks’, I also had to break the news to family, friends and colleagues. Emotionally it was gruelling- picking up the phone and calling people to deliver bad news is never easy. In the end I decided that I couldn’t do it anymore. I had to stop and just send messages. I could only share the information that I had: I have cancer, I’m having an operation and that’s all I can tell you.
I didn’t fixate on my mortality, or my strong desire to avoid chemotherapy. I was realistic, but I also knew that I had to stop obsessing about what I couldn’t change. I just knew that I had to get through this, one step of a time.
Make a plan and have contingencies
In the lead up to my surgery, I thought about the different scenarios and what support our family would need. I did tell my husband that if I died, he had my blessing to take the children to South Africa where some of his family and many friends still live. It was a hard conversation, but it was important for me to talk through the “ifs”. Cancer doesn’t just impact the patient, it is really important that partners/carers access support. Many carers still need to work to bring in an income, and often forgo their own health and personal needs.
Recovery was a rough ride
I would describe my recovery as lengthy. In the first three months, I had three emergency department presentations. I had a collapse, abnormal blood tests and then a severe drug reaction. For 6-7 months I managed daily nausea, extreme fatigue, muscle wasting, weight loss, diarrhoea and dizziness. I had many days of needing to parent from the lounge. I would try to take the boys out each morning to ‘burn off some energy’, but many outings had to be cut short because of my symptoms. I had to become innovative and think of new ways to entertain, which required minimal effort and that were safe. Now when I think back, I can think of new and creative ideas that I could have put into action. When you are so unwell, your motivation and brain power is low. Innovation was limited!
The more unwell I was the more my boys wanted to be held and cuddled. I had to begin sleeping with my 18 month-old because he would no longer sleep by himself and just wanted me. I would surround myself with pillows so he couldn’t kick my stomach accidentally overnight. He would still wake intermittently. My three-year-old then started to wake and my husband spent many nights sleeping on the floor in his room- all while still working, taking over the majority of the household tasks, and caring for me. We were at our absolute limit.
I missed being ‘normal’ and all of the things that I had taken for granted- playing ‘racey tickle’, beach plays, bike rides and even just cleaning up.
Our many meal drop offs from friends and family were godsends. Not having to think about evening meals, as simple as it sounds was such a relief. My boys were too young to be dropped off at friend’s houses for play dates, so our greatest respite came from additional day care hours. We were so lucky to be able to access additional care. We probably should have accessed more, but we did try our hardest to keep life as normal as possible for the boys. Recently the Australian government has released additional funding for in-home childcare for eligible parents link, this is fantastic news and I would encourage parents in need to explore this as an option.
Parents have the greatest motivator to get well
It was after my 3rd emergency department visit that I decided that I really had to change my approach to my recovery. I realised that I was no longer afraid of dying, I was afraid of living as a sick mum. My children were my greatest motivator.
Up until this point, I had ‘controlled’ what I could: my diet, my medications and delegated all that I could. I was seeing multiple health professionals and still I wasn’t getting better in my opinion. I had to focus on what else I could control: my mindset. I began researching the impact on mindset and health and started to make small but important changes. Gratitude lists, meditation, affirmations, visualisations and watching positive Youtube clips all became part of my recovery. In the lead up to my surgery I had begun the daily visualisations of being given “the all clear”. I knew it made me feel good: so I just built on what I had already started.
How Bloomhill helped
Bloomhill is an incredible and unique hub of community cancer care. The team is led by exceptional clinicians who understand the unique ‘at-home’ needs of cancer patients. The support of the Bloomhill team has been pivotal in my recovery. Bloomhill helps to provide clients with essential cancer services after they leave hospital. The nurses, counsellor, exercise physiologist and acupuncturist have all played an important role in my recovery. Having all of these services (and more) under one roof, in a warm and welcoming community environment is fantastic. Their approach to expert and evidence-based cancer-care is renowned in the region and beyond.
It is so important that Bloomhill exists in our community. After cancer treatment, some patients find visiting a hospital very triggering. It is often where we are delivered bad news, receive medications that have side-effects and often a place where we have experienced pain. The experience of being able to be supported in a relaxed, calm, warm and non-clinical environment cannot be put into words.
My boys absolutely love the Bloomhill volunteers who look after them during my appointments. I don’t have to organise or pay for babysitting, they just come with me and we all have an outing. My boys refer to Bloomhill as “mummy’s massage place”. The first time they came with me I had a cancer massage. So the name had stuck!
The Sunshine Coast deserves access to this amazing organisation, for not only current patients, but for members of our community who will walk the cancer journey after us.
Top tips if you’re dealing with a cancer diagnosis
- Link in with a good GP who understands you and your needs. A good GP is so important (It’s up there with quality sleep).
- Ask your questions. Ask lots of questions until you have all the facts and understand your condition, the treatments, and recovery times. There are some great resources at https://www.choosingwisely.org.au/consumers-and-carers to help you have good conversations with healthcare providers.
- Nourish your mind. Make a point of surrounding yourself with positive stories. Develop a daily practice to nourish your mind- meditation, gratitude, journaling (whatever resonates with you). My mindset became my ‘superpower’ and I could only do that by having a lot of counselling and support, which I had at Bloomhill. Bloomhill runs courses on meditation and visualisation (along with Yoga and Tai Chi).
- Accept support. Delegate anything you can. If you have anyone in your circle who is putting their hand up and saying can I help you? Say, ‘yes, fantastic’. Write out a list of tasks you can hand over. Think about your partner as well, we can underestimate the impact the extra responsibilities will have on them.
- Be kind and gentle on yourself. The days (and nights) can be tough and long. Young children may need you more when you are unwell. Be kind to yourself and surrender to timeframe expectations around your recovery.
- Get help from Bloomhill if you haven’t already. You won’t be asked how you are, you’ll be asked, ‘what can we do for you?’